The BAMSE study is a longitudinal, population-based prospective birth cohort including children born 1994-1996 in Stockholm, Sweden, initially designed to study risk factors for allergic disease in childhood.
BAMSE is a population-based longitudinal birth cohort study established in Stockholm in 1994. The overarching goal of BAMSE is to determine the risk factors for asthma and allergies in a population setting.
Specific objectives of the study include:
Newborn children were recruited from child health care centres in four areas of Stockholm: the municipalities Järfälla, Solna, Sundbyberg and northwest parts of the inner city (Norrmalm and Vasastaden) between February 1994 and November 1996. Out of 7,221 children born in the study area during the recruitment period, 5,488 were eligible according to the inclusion criteria. The final cohort consisted of 4,089 children (50.5% boys), i.e., 75% of eligible, whose parents answered a baseline questionnaire when the children were on average two months old. Since its establishment, seven repeated measurements have been performed at 12 months, 2, 4, 8, 12, 16, and 24 years. Recently a COVID-19 follow-up was integrated into the cohort. Data collections in the cohort have been undertaken by means of questionnaires, clinical examinations and linkage to population register data. Example of data types collected include blood samples (for measurement of IgE, DNA, RNA, Blood status, lipids etc.), urine, saliva, nasal samples, lung function (sprimometry, PEF, impulse oscillometry, N2 washout test), FeNO, anthropometrics, body composition, blood pressure, and more. Questionnaire data contain information on allergic disease, environmental factors, lifestyle, diet, sociodemographic factors, etc.
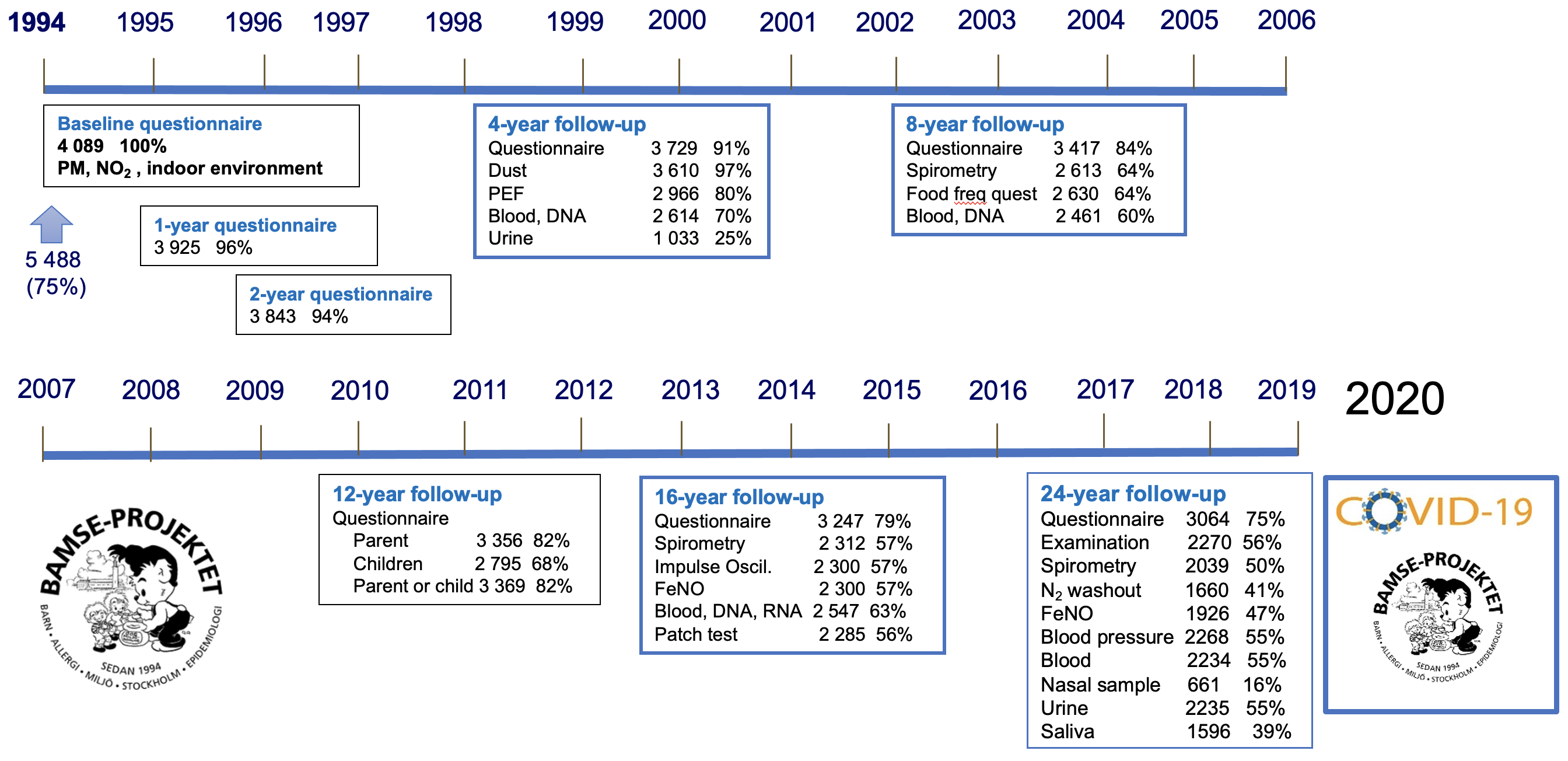
Flow chart of the BAMSE birth cohort for the period 0-24 years.
Anchor: Main sub-projectsChildhood asthma persisting into adult life is associated with long-term lung function deficits and to an increased susceptibility to non-reversible airflow limitation, the hallmark of chronic obstructive pulmonary disease.
This project aims to investigate long-term respiratory and allergy outcomes in relation to early life disease, environmental exposure, and genetic/epigenetic factors.
Specific aims include:
Research Group Melén
Sophia Björkander, Assistant Prof, PhD
Susanna Klevebro, MD, PhD, Assoc. Prof.
Jenny Hallberg, PhD/Assoc. Prof
Petra Um-Bergström, MD, PhD, researcher
Gang Wang, MD, PhD, postdoc
Shizhen He, PhD postdoc
Simon Kebede Merid, PhD
Ashish Kumar, statistician
Björn Lundberg, MD, PhD
Maura Kere, MD, PhD student
Zhebin Yu, Assistant Prof, PhD (Group Gruzieva)
Asthma is a complex disease characterized by recurrent episodes of airway hyperresponsiveness and reversible airflow obstruction. Clinically, asthma is often sub-grouped into allergic asthma that requires sensitization to a relevant allergen, and non-allergic asthma defined by a lack of coincidental sensitization. Few studies have identified immunological features and biomarkers beyond sensitization, exhaled NO (FeNO) and blood counts that distinguish asthma subtypes. Extensive investigation of type 2 (T2) plasma biomarkers and the immune system may aid diagnostics and help tailor disease treatment in a precision medicine manner.
The aim is to use large-scale analysis of inflammatory-related plasma protein biomarkers and extensive immune phenotyping (CyTOF and innate lymphoid cells, ILC cytometry) to perform characterization of asthma phenotypes in young adults. In addition, genetic data will be used to explore mechanisms and causal pathways. Identified biomarkers and immunological signatures are analyzed in combination with established clinical read-outs (FeNO, IgE, lung function, blood eosinophils).
Research Group Melén
Sophia Björkander, Assistant Prof, PhD
Susanna Klevebro, MD, PhD, Assoc. Prof.
Jenny Hallberg, PhD/Assoc. Prof
Petra Um-Bergström, MD, PhD, researcher
Gang Wang, MD, PhD, postdoc
Shizhen He, PhD postdoc
Simon Kebede Merid, PhD
Ashish Kumar, statistician
Björn Lundberg, MD, PhD
Maura Kere, MD, PhD student
Zhebin Yu, Assistant Prof, PhD (Group Gruzieva)
Dietary factors such as antioxidants and fatty acids have been hypothesized to influence the development of asthma, but the results from previous studies are conflicting. Recent findings from the research group indicate that diet (intake of fish, polyunsaturated fatty acids and antioxidants) in school age may influence asthma up to adolescence, and that diet may influence lung function development among children with asthma. However, it remains unclear how dietary patterns and other dietary factors (e.g. dietary fibre) influence asthma and lung function development. Furthermore, development of asthma is a dynamic process, and the role of diet for development of asthma up to adulthood remains unknown. There are few longitudinal cohorts with repeated information on diet, asthma and lung function from childhood to adulthood. Since dietary habits may change over life, having measures of diet at different ages is a major advantage in studies on diet and subsequent asthma and lung function.
Diet is also a major determinant of cardiometabolic disease in adulthood, and the types of fatty acids consumed have been considered to play an important role. However, evidence from studies on children and adolescents are limited and few prospective studies have monitored diet from childhood to adulthood using objective biomarkers of diet, including fatty acid intake.
Tobacco exposure is an important determinant of health. Still, we need to better understand how exposure in fetal life, childhood and adolescence influence health in adulthood. Results from the group show that second hand tobacco smoke in early life and diet in school age influence the development of allergic diseases up to adolescence. Recent results indicate that smoking in adolescence is associated with lung function impairments at age 16 years. However, it remains unknown if the changes persist to adulthood.
The aim of the proposed project is to gain further knowledge on the role of second-hand smoke exposure, cigarette smoking, snus consumption and diet for health outcomes in young adults, and to provide a basis for disease prevention efforts.
Specific aims:
Adolescence and young adulthood are challenging phases in life, particularly when compounded with a chronic disease. One of the most common chronic diseases is asthma, which has an estimated prevalence of 12–14% in adolescence and young adulthood. Living with asthma implies a substantial disease burden. Among those aged ≤ 20 years, asthma was ranked eighth out of 369 diseases and injuries as regards impact, measured as years lived with disability. Asthma annually accounts for the loss of over 15 million disability-adjusted life years (DALYs) and ranks among the most common causes of DALYs in children.
It is known that living with asthma in adolescence is associated with impaired health-related quality of life (HRQoL), which is more pronounced if the asthma is uncontrolled. However, how the transition from paediatric to adult healthcare affects HRQoL is unclear. Using data from our population-based cohort, we have recently investigated HRQoL among young adults with asthma during the transition process. Further, we assessed if asthma control and physical activity influenced the potential association. Preliminary results showed that HRQoL, measured with a generic instrument, was lower in young adulthood than in adolescence. This was more pronounced in young adults with uncontrolled asthma or who were physically inactive.
The overall aim is to identify factors of importance for improved care of children and young people with allergic disease, with a special focus on the transition from childhood to adulthood.

Karolinska Institutet and Region Stockholm.
Anchor: CollaboratorsWe welcome potential collaborators to any of our sub-projects. Please contact the project leaders for sub-project you are interested in or write to any of the contact persons below.
Anchor: contactsWickman M, Kull I, Pershagen G, Nordvall L. The BAMSE project: presentation of a prospective longitudinal birth cohort study. Pediatr Allergy Immunol.
Ballardini N, Kull I, Lind T, Hallner E, Almqvist C, Ostblom E, Melén E, Pershagen G, Lilja G, Bergström A, Wickman M. Development and comorbidity of eczema, asthma and rhinitis to age 12: data from the BAMSE birth cohort. Allergy 2012;67(4):537-44.
Melén E, Bergström A, Kull I, Almqvist C, Andersson N, Asarnoj A, Borres MP, Georgellis A, Pershagen G, Westman M, van Hage M, Ballardini N. Male sex is strongly associated with IgE-sensitization to airborne but not food allergens: results up to age 24 years from the BAMSE birth cohort. Clin Transl Allergy. 2020;10:15.
Björkander S, Du L, Zuo F, Ekström S, Wang Y, Wan H, Sherina N, Schoutens L, Andréll J, Andersson N, Georgelis A, Bergström A, Marcotte H, Kull I, Hammarström L, Melén E, Pan-Hammarström Q; BAMSE COVID-19 study group. SARS-CoV-2-specific B- and T-cell immunity in a population-based study of young Swedish adults. J Allergy Clin Immunol. 2022 Jan;149(1):65-75.e8. doi: 10.1016/j.jaci.2021.10.014. Epub 2021 Oct 23.
Wang G, Kull I, Bergström A, Hallberg J, Bergström PU, Guerra S, Pershagen G, Gruzieva O, van Hage M, Georgelis A, Janson C, Lindén A, Melén E. Early-life risk factors for reversible and irreversible airflow limitation in young adults: Findings from the BAMSE birth cohort. Thorax. 2021 May;76(5):503-507.
Thacher J, Gruzieva O, Pershagen G, Neuman A, Wickman M, Kull I, Melén E, Bergstrom A. Pre- and Postnatal Exposure to Parental Smoking and Allergic Disease Through Adolescence. Pediatrics 2014;134:428-34.
Ödling M, Andersson N, Hallberg J, Almqvist C, Janson C, Bergström A, Melén E, Kull I. A gap between asthma guidelines and management for adolescents and young adults. J Allergy Clin Immunol Pract. 2020 Jun 6:S2213-2198(20)30530-4.
For more publications, please visit: https://ki.se/en/imm/bamse-publications
Anchor: links